IR Information
FAQ
Company Profile
- What is the origin of the company name?
-
創業者は腎臓専門医ですが、創業当時は腎臓病の治療薬はほとんどありませんでした。当社は腎臓病の治療薬の開発を目的に設立されたため、「腎臓+科学」を意味する「レナサイエンス」と名付けられました。レナサイエンスには「復興」や「再生」という意味もあります。
医薬品は必ずしも必要とされる医療分野で開発されているわけではなく、腎臓疾患(有効性の評価に時間がかかることから医薬品開発が難しい疾患)や希少疾患(患者数が少なく売上が少ない疾患)などの領域における医薬品開発は遅れています。そこで当社は現在、開発困難な治療領域や希少疾患における医薬品開発に積極的に取り組んでいます。
- Where are your business locations?
-
本社は仙台(宮城県)にあり、研究開発センターは東北大学大学院医学系研究科附属メディカルハブ(宮城県仙台市青葉区星陵町2-1 医学部5号館)にあります。
- What are the reasons for developing various modalities (therapeutic technologies)?
-
私たちは、医療上の問題を解決し、人類が心身ともに生涯健康でいられるような新しい治療法を創りたいと考えています。私たちは特定の技術に特化したバイオテクノロジー企業ではないので、どんな治療法でも構いません。
製薬業界は、従来の低分子医薬品の開発からバイオ医薬品の開発へと多様化が進んでいます。さらに、近年の工学技術や情報技術の進歩により、情報技術と工学技術を融合した新たな医療の模索が進んでおり、欧米や日本の大手製薬企業はすでに医薬品のみのビジネスから医療ソリューションビジネスへとシフトしています。医療における治療の選択肢は、医薬品、医療機器、さらには医療機器としてのソフトウェアや人工知能(AI)を活用したアプリケーションまで広がっています。
そのため、当社は、これまで注力してきた化学・生物学研究に加え、工学・情報研究へと視野を広げ、多様で魅力的な研究・事業ポートフォリオを構築したいと考えています。
- What medical issues are you working on?
-
世界保健機関(WHO)は、加齢や生活習慣に関連する重要な疾患(加齢関連疾患)を「非感染性疾患(NCD)」と定義し、がん、糖尿病、呼吸器疾患、心血管疾患の4つの疾患領域を対象としています。これらの疾患は、2023年には世界の全死亡数の74%を占めています。当社の開発品目は、これら4つの疾患領域すべてを対象としています。
もう一つの重要な社会課題は少子化ですが、少子化問題に着目している製薬会社は多くありません。当社は、女性特有の医療課題(月経前不快気分障害、更年期障害、乳がんのAI診断)や小児疾患(フェニルケトン尿症の迅速診断)に注力しています。
- What are your reasons for emphasizing collaboration with outside research and medical institutions?
-
医療イノベーション創出における大学や医療機関などの公的研究機関の役割は拡大しています。従来の低分子合成医薬品とは異なり、遺伝子工学技術などを活用したバイオ医薬品は、技術基盤やシーズが大学などの公的研究機関に帰属します。また、人工知能(AI)を活用した医療機器のソフトウェア開発に必要な医療データも医療機関が保有しています。
レナサイエンスは、多くの医療機関の複数の科と連携して医師主導治験を実施しているため、医療現場の課題を把握する機会が多く、AI開発に必要な医療データも比較的短期間で容易に取得できます。自社のリソースや研究環境に固執するのではなく、外部のリソースや外部環境を積極的に活用し、効率的なイノベーションの仕組みを構築することに重点を置いています。
- What are the advantages of developing a product from basic research to investigator-initiated clinical trials in one integrated process?
-
基礎研究から治療のコンセプトやアイデアを構想し、医薬品や医療機器を「創る」。そして、適切な動物や細胞を用いた非臨床試験を終え、必要な臨床試験(治験)で有効性や安全性を実証。薬事承認申請に近いところまで自社で開発し、販売許可を取得したいと考えています。
例えば、2022年12月に承認を取得した医療機器(極細内視鏡)は、複数の大学と連携し、製品づくりから非臨床試験、臨床試験(製品の研究を行った医師が行う医師主導治験)まで行い、海外の医療機器企業に導出後、薬事承認申請しました。また、現在、血液がんの一種である慢性骨髄性白血病の治療薬として、承認申請に必要な最後の臨床試験である第Ⅲ相試験を実施しており、他の希少疾患についても引き続き第Ⅲ相試験を自社で実施していく予定です。その理由は、大手製薬企業が希少疾患の薬に注力することが難しい場合があるからです。
自社で承認まで開発することで、重要なシーズを確実に社会実装できるとともに、開発後期段階で導出することでより大きな対価を得ることができ、株主への還元も可能になると考えています。
- What is the reason why you can develop the products all the way from basic research to investigator-initiated clinical trials?
-
当院では、基礎研究から臨床試験まで幅広い研究を行っている医師(フィジシャン・サイエンティスト)との共同研究を重視しています。つまり、当院と共同で基礎研究を行う研究者は医師であり、医師主導臨床試験では調整研究者(治験責任医師)として実施することができます。このように、基礎研究と臨床研究を行う研究者は同一であることが多く、基礎研究と医師主導臨床試験を一体的に進め、効率的な開発を進めることができます。
- What are the advantages of the open innovation?
-
従来、多くの製薬企業や創薬バイオテック企業は、パイプラインバリューチェーン(開発プロセス全体の積み重ね)全体を自社で構築することで、事業価値を高めることに注力してきました。しかし、医薬品のように成功確率が極めて低く、開発期間が長く、投資額が大きい分野では、研究開発リスクや事業リスクが高く、多くのパイプラインを組み合わせたポートフォリオを形成し、リスクを分散させることが不可欠です。豊富な資金を背景に持つ大手製薬企業であれば、自社でバリューチェーンを形成するという既存の枠組みの中でパイプラインを開発できる場合が多いですが、バイオテック企業のように資金が豊富でない場合は難しいのが現状です。
当社は、外部機関(研究機関、医療機関)のリソースを活用することで、コストを含めた開発効率の高い開発を実践しています。当社は、外部機関とのアライアンスによるバリューチェーンの構築を多く考えており、既存のバイオベンチャーとは異なる戦略、研究開発、人材マネジメントを行っています。より少ない社内人材と経費で、多くのパイプラインの拡充やモダリティ開発を行っており、その成果も出始めています。当社は、自社のリソースや社内環境だけに注力するのではなく、外部リソースや外部環境を積極的に活用し、効率的なイノベーションの仕組みを構築したいと考えています。大学や異業種企業との提携・連携によるオープンイノベーションを推進し、効率的にパイプラインの開発を行っています。
- Why did you establish the Tohoku University Renascience Open Innovation Labo (TREx) and Hiroshima University Renascience Open Innovation Labo (HiREx)?
-
2022年1月、東北大学大学院医学系研究科メディカルハブ(宮城県仙台市青葉区星稜町2-1 医学部5号館)内に「東北大学ルナサイエンスオープンイノベーションラボ(東北大学×ルナサイエンス=TREx)」を開設しました。
レナサイエンスは創業当時、神奈川県川崎バイオテクノロジー特区内に腎臓病モデル動物の飼育施設を含む研究所を構えていました。その後、腎臓病から他の疾患領域へと研究対象が広がり、研究段階も基礎から臨床試験へと進むにつれ、腎臓病モデル動物を主力としていた当初の研究所は閉鎖されましたが、多くの疾患領域における最先端の科学技術成果を活用する「場」、医師や研究者と直接交流する「場」、行政や医療産業企業とのオープンイノベーションの「場」が必要であると考え、TRExを開設することとしました。
TRExは、2021年4月に締結した「仙台市と東北大学との地域経済活性化に関する協定」に基づく第1弾の拠点立地事業です。TRExの設立により、1)東北大学大学院医学系研究科の研究者、東北大学病院の医師、メディカルハブ参画企業、行政機関などの異分野連携の加速、2)既存開発パイプラインの研究推進と複数の新規シーズの導入、3)医師主導治験、医療データへのアクセス、公的資金の獲得、ライセンス戦略立案などを効率的かつ迅速に実施、4)人材の育成・確保が可能となり、当社の強みである研究開発の高効率化をさらに加速することが可能となりました。
2023年4月には広島大学と包括連携協定を締結し、TRExに続き広島大学ルナサイエンスオープンイノベーションラボ(広島大学×ルナサイエンス=HiREx)を設立しました。HiRExを活用し、非小細胞肺がんや皮膚血管肉腫などの医薬品の医師主導治験や、糖尿病治療支援や維持透析医療支援など人工知能(AI)を活用した医療機器(SaMD)としての各種ソフトウェアの臨床性能試験を実施します。
- Why do you place importance on obtaining public research funding?
-
医薬品の研究開発、特に臨床試験には多額の研究開発費が必要です。当社は医師主導治験によりシーズを開発し、製薬企業にライセンスアウトするビジネスモデルであるため、多額の研究開発費を自ら負担する必要があります。
しかしながら、公的研究費(競争的研究資金)を積極的に活用することで、こうしたリスクの高い医師主導治験に要する自社の研究開発費を削減することが可能となります。当社は今後も公的研究費を積極的に獲得し、活用してまいります。
- What are the results of the transition to a company with an Audit and Supervisory Committee?
-
当社は、効率的かつ迅速な経営判断を行うために、また、当社の規模に鑑み、最適なガバナンス体制を検討した結果、監査等委員会設置会社を導入することが適切であると判断し、組織設計を変更しました。これにより、社外取締役の客観的な意見を意思決定に反映させ、これまで以上に透明性の高い経営を行うことができると考えております。
Presentation/Outside Activities
- Does Renascience do any social activities?
-
少子化は重要な社会課題であり、当社は女性(月経前不快気分障害、更年期障害、乳がんのAI診断)や子ども(フェニルケトン尿症の迅速診断)の医療課題に注力しており、子どもや女性の社会活動を支援することが当社の社会的責任(CSR)であると考えています。下記具体例に加え、子どもや女性の健康のための啓発活動も支援していきます。
- Please tell us about your latest academic activities.
-
□ Lecture on “Development of a machine learning model that suggests frequent insulin injection treatments mimicking those of diabetes specialists”
・May 19, 2024 67th Annual Meeting of the Japan Diabetes Society
At the 67th Annual Meeting of the Japan Diabetes Society (date: May 19, 2024, venue: Tokyo International Forum), Assistant Professor Kei Takahashi of the Department of Diabetes and Metabolic Medicine, Tohoku University Graduate School of Medicine, gave a lecture titled “Development of a machine learning model that proposes frequent insulin injection therapy that mimics the instructions of diabetes specialists.”□ Special lecture on “Clinical application of PAI-1 inhibitors”
・October 18, 2024: 31st Autumn Symposium of the Japan Society of Transfusion Medicine and Cell Therapy
At the 31st Japan Society of Transfusion Medicine and Cell Therapy (date: October 18-19, 2024, venue: Sonic City), Professor Toshio Miyata (Chairman of the Board of Directors of our company) of the Tohoku University Graduate School of Medicine gave a special lecture on “Clinical Applications of PAI-1 Inhibitors.” He spoke about the new role of PAI-1 in cancer and aging, and the research and development status of PAI-1 inhibitors as a treatment for these diseases.□ Lecture on “Creating Medical Innovation: Expanding the Role of Academia and Changing Research Environments”
・May 27, 2025: Sapporo Medical University 1st Startup Seminar
At the 1st Sapporo Medical University Startup Seminar (date: May 27, 2025, venue: Sapporo Medical University), Professor Toshio Miyata (Chairman of the Board of Directors of our company) of the Tohoku University Graduate School of Medicine gave a lecture on the theme of “Toward the Creation of Medical Innovation: The Expanding Role of Academia and the Changes in the Research Environment.” With the development of science and technology in recent years, the role of academia has also expanded.These include biopharmaceutical development, artificial intelligence that utilizes medical big data, investigator-initiated clinical trials, and even startup launches for practical application. We hope that this seminar will provide an opportunity to consider the university research environment necessary for these areas.
Development Pipeline
- What is important to increase the probability of success in drug development?
-
新薬開発においては、候補薬の安全性と有効性を確認することが重要です。安全性は、一般毒性や遺伝毒性などの薬事法規に則った試験で評価することができ、試験には適切な時間と費用をかけて実施することができます。一方、有効性の評価はそれほど簡単ではなく、どの疾患に薬が効くのかを見極めるのは困難な作業です。
本来の適応疾患に効果がない薬剤でも、別の疾患には効果がある場合があります。ある薬剤に対して幅広い適応症を考慮すること(ドラッグ・リポジショニング)は難しく、すべての疾患に対して薬剤を考慮することは事実上不可能です。
当社は、国内外の公的研究機関に所属する研究者に対し、当社のパイプライン化合物を「オープンリソース」として提供しています。最先端の基礎研究を行っている各分野の研究者と連携できる体制により、限られた自社のリソースのみで基礎研究を進める場合に比べ、はるかに効率的かつ広範囲なドラッグリポジショニング研究を進めることが可能です。
- What are the advantages of investigator-initiated clinical trials?
-
当社の臨床試験は、研究者であると同時に医師でもある医師科学者によって研究者主導で実施されます。
医師主導治験の圧倒的なメリットは「質」と「スピード」、つまり「効率」です。医師主導治験では、研究の最前線にいて、最新の研究成果にアクセスでき、医療現場で日々患者さんを診ている医師が、適切な患者集団や研究計画を立案することができます。医師自らが治験を実施できるため、未承認薬の早期治験(薬の有用性や安全性を初めて確認する段階、探索的治験と呼ばれる)には適した治験の枠組みです。また、希少疾患(患者数が少なく、大きな売上が見込めない疾患)は、製薬企業が収益性が低いため、医薬品開発に取り組まないケースが多く、最初から最後まで医師主導治験で実施しなければならない場合もあります。研究開発費の大半は、基礎研究段階ではなく、臨床開発段階に費やされています。
医師主導治験は、大学等の先端科学技術の成果を迅速に活用できること、治験責任医師が適切に治療対象患者を選択できることから、開発コストの削減が可能です。他社とは異なり、適切な治験責任医師を指名し、大学等の複数の大規模医療機関の支援が得られる場合、医師主導治験は企業主導治験に比べて大きな利点があり、短期間で大規模な治験を実施できるため、当社はこの治験形態を優先しています。
- Aren't investigator-initiated clinical trials for the expansion of indications for drugs approved overseas (but not yet approved in Japan) or existing drugs?
-
2003年の薬事法改正により、医師自らが治験を実施する「医師主導治験」が可能となりましたが、安全性試験や薬剤処方など、治験に必要な薬剤を全て医師自ら準備することは依然として困難です。
法改正当時は、海外では承認されているが国内では未承認の新薬や適応外の新薬(いわゆるドラッグ・ラグ)が多かったため、医師主導治験は国内未承認薬や適応外薬の適応拡大が主な対象であった。治験の実施しやすさ(製造から安全性試験まで既存データを活用できる)の観点から、大学を含む医療機関の医師の多くが、海外で承認されている(国内未承認)新薬や適応外薬の医師主導治験を実施していた。また、製薬企業が手掛けていない希少疾病の既存薬を用いて医師主導治験を実施するケースもあった。こうした背景から、医師主導治験は海外で承認されている(国内未承認)薬や既存薬の適応拡大という印象が依然として強いように思われる。
ただし、当社が実施する臨床試験は、すべて未承認薬(ヒト初)の臨床試験であり、海外で承認されている薬(国内未承認)や既存薬の適応拡大を目的とした臨床試験ではありません。当社が実施する医薬品は未承認薬であり、知的財産権を確保しているため、独占的に事業化することができ、十分な利益を得ることができます。
- Is it possible to apply for regulatory approval with the results of investigator-initiated clinical trials?
-
当社の医薬品開発においては、非臨床試験は医薬品の安全性および有効性の試験実施基準(GLP)に準拠して実施され、治験薬の製造は治験薬の製造管理および品質管理の基準(GMP)に準拠して行われています。また、医師主導治験は、企業主導治験と同様にGCP(医薬品の臨床試験の実施基準)に準拠して行われています。そのため、医師主導治験の結果は、薬事申請や薬事承認取得に活用することができます。
- What are the reasons for the large number of drugs in your pipeline?
-
当社では、開発化合物を国内外の大学等の公的研究機関の研究者にオープンリソースとして提供し、当社医薬品の適応拡大の可能性について多岐にわたる検討(ドラッグ・リポジショニング)を効率的に進めることで、数多くの医薬品のパイプラインを拡充することに成功しています。
臨床開発候補とならない化合物についてはマテリアルトランスファー契約(MTA)を、臨床開発候補となる化合物についてはコラボレーション契約(研究開発の実施許諾、新発見の知的財産の取り扱い、事業化後の補償を含む契約)を締結し、提供しています。創業以来、MTAで提供した化合物をオープンリソースとして、100を超える研究機関が当社のプロジェクトに取り組んでいます。国内外の数多くのコラボレーションから、自分たちでは思いつかなかったシーズ(発想)が生まれています。
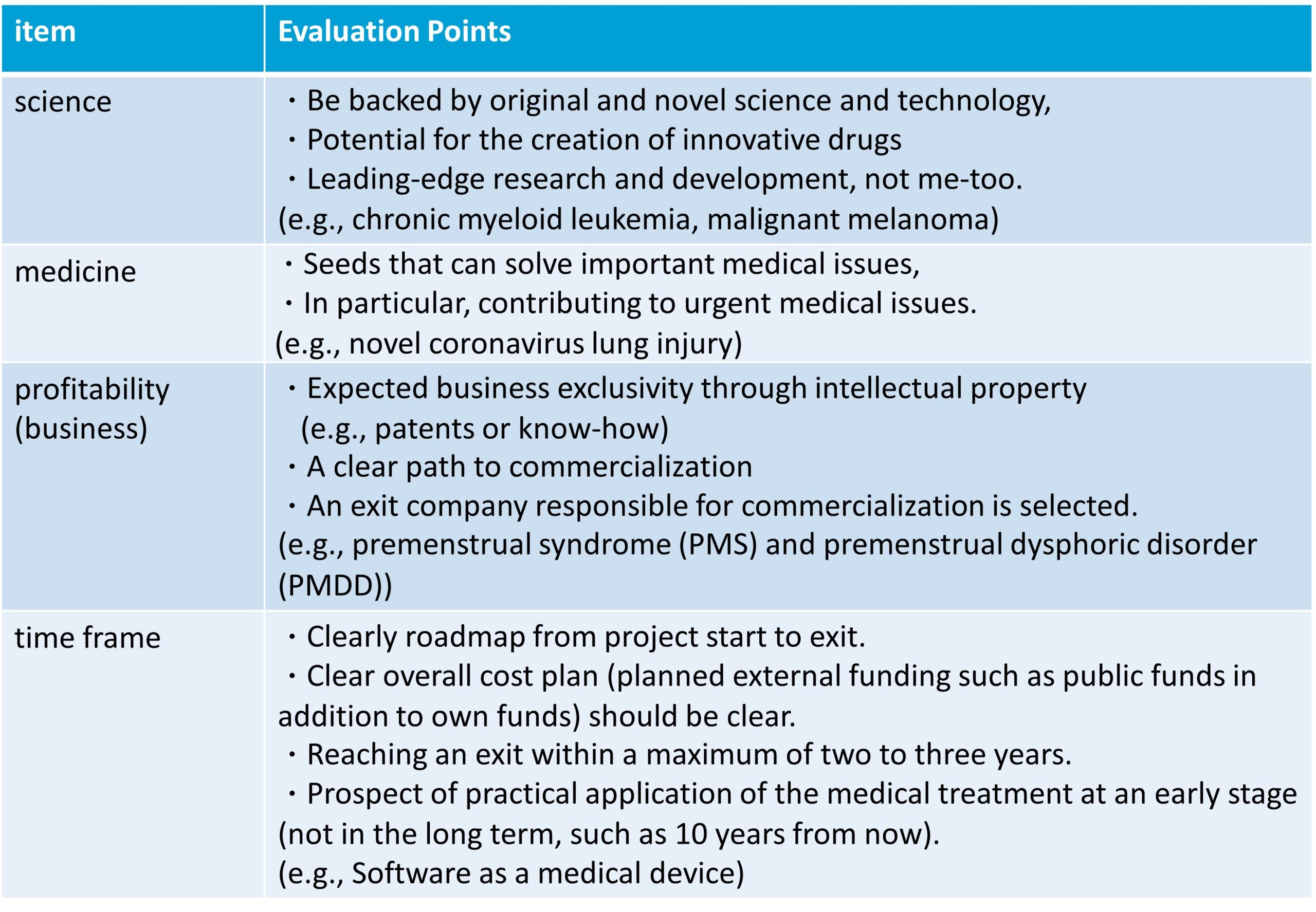
- What kind of criteria do you have when deciding on pipeline development?
-
当社では、下表の科学、医学、収益性(ビジネス)、時間枠の 4 つの要素を総合的に考慮してパイプライン開発の決定を行っています。
- What are your considerations regarding intellectual property?
-
当社は大学等の公的研究機関と連携しているため、知的財産は大学等との共同出願(特許の共同出願)が基本となります。大学等の職務発明規程を遵守しつつ、大学の産学連携担当部門(知的財産部)と協議を重ね、大学等の社内規定に則った知的財産出願・管理・運用が必要となります。また、知的財産の出願は、発明者、出願人、権利帰属割合、費用負担、ライセンス条件(範囲、対価)等について合意した上で行います。これらの交渉・合意には相当の期間(数ヶ月)を要するため、これらの期間を考慮した知的財産出願計画を策定する必要があります。
物質特許のみならず、用途特許、剤形特許など複数の関連特許を適切かつ継続的に出願・維持・管理しています。
- Why are you able to conduct many collaborative projects with university researchers?
-
当社では、国内外の公的研究機関に所属する研究者に対し、化合物をオープンリソースとして提供しています。
公的研究機関の研究者の研究室には、専門分野の研究設備や独自の疾患モデル動物がありますが、医学や生物学を専門とする研究者には薬の候補となる化合物がありません。レナサイエンスのオープンリソースポリシーにより、これらの化合物の情報を知った国内外の多くの研究者から依頼が増えています。特許出願後は、協力者には学会や論文で自由に発表してもらえるほか、当社の化合物をもとにした研究資金の申請も認めてもらえることになりました。
最先端の基礎研究を行っている研究者と共同で化合物開発を進める当社の体制は、限られた自社のリソースのみで基礎研究を進めるよりもはるかに効率的で広範囲にわたります。
- What are the advantages in research and development of software as a medical device (SaMD) utilizing artificial intelligence (AI)?
-
人工知能(AI)の医療分野への応用は大きな可能性を秘めたテーマですが、医療AIの研究開発において重要な役割を担う関係者はそれぞれ課題に直面しています。
医師(医療機関)は医療の課題や問題点(ニーズ)に精通し、医療データやアイデアも豊富であるものの、AI技術やITベンダーとのネットワークが不足しており、具体的な研究開発プロジェクトを立ち上げることが困難となっています。一方、AI技術を有するITベンダーは、成長が見込まれる医療分野への応用に関心はあるものの、医師(医療機関)とのネットワークが少なく医療ニーズや医療データへのアクセスが困難であること、薬機法をはじめとする薬事行政や規制に関する経験が不足していることなどから、実用化は容易ではありません。また、AIの医療応用を事業化したい出口の製薬企業やヘルステック企業も、研究から事業開発まで全てを自社で行うのは時間やリソースの面で難しい場合が多いです。
そのため、医療課題を知り尽くした医師(医療機関)、AI技術を有するITベンダー、出口となる製薬・ヘルステック企業が最初から連携し、AIを活用したソフトウェアの医療機器としての開発を推進できる体制が重要となります。そのためには、開発の初期段階から薬事承認や出口、実際の臨床実装を見据えた計画が不可欠です。そのためには異分野間のオープンイノベーションが重要であり、医師だけでなく、データサイエンティスト、AI研究者、薬事専門家などが連携して取り組む必要があります。
レナサイエンスは、数多くの医師主導治験を実施する過程で、多数の医療機関や複数の診療科とのネットワークを構築し、医療課題や医療データへの容易なアクセス(医療支援)、オープンイノベーションによる複数のIT企業との協業業務契約の締結(技術支援)、医薬品の医師主導治験の実施過程における薬事規制への対応などを実現しています。
- What are the important aspects of medical applications of artificial intelligence (AI)?
-
医療AIの研究開発には、1)医療課題、2)医療データ(質・量)、3)AIアルゴリズム(エンジン)の3つの要素が必須となりますが、優れた技術であっても、医療現場のニーズに合致せず、医療現場で活用するには課題があるため実用化が難しい場合が多く、技術を保有する多くの企業がその課題に直面しています。
近年、医療現場のニーズから課題解決法を考案し、医療現場の最終製品を想定して最適化する「バイオデザイン」という手法が注目されています。AIをコア技術とする医療機器などのソフトウェアにも同様の手法が応用できますが、AI技術はもちろん重要ですが、医療データは機械からではなく個人差のある患者から得られるものであることに注意が必要です。そのため、医療現場の課題や医療データ、医師のアドバイスをもとにAIをカスタマイズすることが重要です。AI研究に欠かせない材料は医療データであり、AIは大量のデータからルールを見つける(帰納的推論)ため、十分な量のデータが絶対に必要です。データの量だけでなく、データの質も重要です。
さらに、解決すべき医療問題や活用する医療データの種類に応じて、最適なAIアルゴリズムを選択する必要があります。特定のAIアルゴリズムが活用できる医療分野を探すのではなく、特定の医療問題を解決するために「最適なAIアルゴリズムを選択(場合によっては独自に開発)」する必要があります。また、AIアルゴリズムが決定した後は、データサイエンティストはデータさえあればAIで解析できますが、その結果が正しいかどうかを解釈・評価できるのは医師だけです。そのため、医師の関与がなければ、良質な医療データを使ってAIを訓練し、問題を解決することはできません。
医師、データサイエンティスト、AI研究者の連携が重要であり、医療課題、医療データ、経験、知識が存在する医療現場(医師)の積極的な関与が、AIによる医療課題の解決を成功させる鍵となります。
当社は、AIの医療応用に関する研究開発を推進するため、2022年11月にNECソリューションイノベータと覚書(MOU)、2023年6月にNECと包括的協業契約(MOU)を締結しました。
- How many pipelines are appropriate for the size of the company?
-
当社では、開発した化合物を国内外の大学や公的研究機関の研究者にオープンリソースとして提供することで、限られたリソースの中で、医薬品の適応拡大(ドラッグ・リポジショニング)の可能性について、多岐にわたる研究を効率的に進めています。また、特定の社内リソースを必要としないため、非臨床試験(疾患モデル動物を用いた試験)の件数に制限はありません。臨床開発は医師主導治験を活用し、CRO(医薬品開発業務受託機関)を活用することで、社内の人材リソースを削減しています。
2022年度の臨床試験件数は7件、2023年度は9件、2024年度は10件(うち臨床性能試験2件)と、徐々に増加傾向にあります。
当社は、年間5件以上の医師主導治験の実施を目標としています。人工知能(AI)を活用した医療機器ソフトウェア(SaMD)については、当社のリソースを踏まえると、探索レベルで年間10件程度のシーズ開発が適正数と考えています。このうち、約30%が開発・事業化レベル(臨床性能試験などの治験の実施)に移行すると考えています。
- What is your current priority among the pipelines?
-
臨床段階が進んでいるパイプラインの開発は最優先事項です。
医薬品分野では、がん領域と呼吸器領域におけるプラスミノーゲン活性化因子阻害剤-1(PAI-1)阻害剤の開発に注力しています。がん領域では、慢性骨髄性白血病の第III相試験が進行中、悪性黒色腫の第II相試験が終了し、非小細胞肺がん、皮膚血管肉腫を対象にした臨床試験を実施しています。呼吸器領域では、新型コロナウイルス肺障害の第II相試験が終了し、全身性強皮症に伴う間質性肺疾患の第II相試験を実施しています。
医療機器(極細内視鏡)の開発はほぼ完了しています。極細内視鏡の本体であるファイバースコープは2022年12月に承認されており、付属部品であるガイドカテーテルの開発もほぼ完了しており、今後は薬事申請に向けた準備を進める予定です。
人工知能(AI)を活用した医療用ソフトウェア(SaMD)については、糖尿病治療支援用SaMDや維持透析支援用SaMDの開発がSaMDプロジェクトの中で先行しており、これらSaMDの臨床性能試験を実施し、薬事承認申請を行う予定です。
- What is the reason for developing the PAI-1 ihhibitor in respiratory disease?
-
PAI-1は血栓の線溶に必要なタンパク質ですが、炎症や組織の線維化にも深く関わっています。これらの作用をもとに、当社は呼吸器疾患を対象としたPAI-1阻害剤の開発を進めています。具体的には、新型コロナウイルス肺障害(第II相試験終了)、全身性強皮症に伴う間質性肺疾患(第II相試験)、間質性肺炎(非臨床試験)などのプロジェクトが進行中です。
- What is the reason for developing the PAI-1 inhibitor in oncology?
-
PAI-1の発現が高いがんは悪性度が高く、予後が悪いことが知られています(「PAI-1パラドックス」)。私たちの共同研究で、PAI-1ががん細胞における免疫チェックポイント分子(PD-L1など)の発現を促進することを発見しました。また、大腸がんと悪性黒色腫のマウスモデルにおいて、私たちのPAI-1阻害剤の投与により、がん細胞における免疫チェックポイント分子の発現が減少し、腫瘍内の細胞傷害性T細胞の浸潤が増加し、腫瘍関連マクロファージが抑制されることも示しました。
これらの非臨床試験の結果をもとに、悪性黒色腫を対象とした第II相臨床試験が実施され、期待される有効性のエビデンスが得られました。ニボルマブに抵抗性の悪性黒色腫患者にニボルマブとRS5614を8週間投与したところ、奏効率は24.1%(7/29例)で、ニボルマブとイピリムマブの既存の奏効率(日本での13.5%)よりも高くなりました。非小細胞肺がん、皮膚血管肉腫を対象に第II相医師主導臨床試験が行われています。がん治療には実際に「PAI-1パラドックス」が関与しており、一部のがん種ではPAI-1阻害剤と他の抗がん剤の併用が相乗的に有効であることが確認されています。
- How was the PAI-1 inhibitor obtained?
-
ヒトPAI-1分子の結晶構造を基に、コンピュータ工学を駆使した約200万の仮想化合物ライブラリの検索から、96のPAI-1阻害候補化合物を得ました。PAI-1活性阻害を指標として、10年以上かけて現在までに1,400を超える新規阻害化合物を合成し、薬効スクリーニングを行いました。さらに化合物の有効性と安全性を評価することで、経口投与可能で安全性プロファイルに優れたリード化合物RS5275を得ました。RS5275からさらに新規化合物を合成し、RS5441、RS5484、RS5509、RS5614の4つの臨床候補化合物を得ました。その中で、RS5614が最終的に臨床開発の候補化合物として選定されました。
- How is the status of domestic and international competition for PAI-1 inhibitor development?
-
これまで、国内外の大手製薬企業を含む多くの製薬企業やバイオテクノロジー企業が、低分子PAI-1阻害剤の開発に取り組んできた。マウスやラットの動物モデルではいくつかの薬剤が効果があると報告され、そのうちPAI-749(ディアプラシニン)は臨床段階まで進んだが、効果が見られなかったため、第1相臨床試験後に開発が中止された。
- Are there any safety issues with the PAI-1 inhibitor?
-
非臨床試験として、安全性薬理試験(hERG試験、ラット中枢神経系、サル心血管・呼吸器試験)、一般毒性試験(ラット26週間経口反復投与試験、サル39週間経口反復投与試験)、遺伝毒性試験、光毒性試験、生殖発生毒性試験などを実施し、臨床試験や薬事申請に問題がないことを確認しています。第I相単回投与試験では、RS5614を240mgまで投与しても安全であることが確認されており、第I相経口反復投与試験では、120mgを7日間投与した際に発現した有害事象はすべて軽度でした。RS5614は、200名を超える被験者(健常ボランティア、慢性骨髄性白血病、新型コロナウイルス肺障害、悪性黒色腫)に投与されています。慢性骨髄性白血病では、33人の患者に1日180mgを48週間投与し、治験薬に関連する重篤な有害事象は報告されなかったため、RS5614は安全な薬剤であると考えられます。
- What is the reason for developing the PAI-1 inhibitor in chronic myeloid leukemia (CML)?
-
慢性骨髄性白血病(CML)は血液がんの一種で、造血幹細胞の染色体の異常によって発生し、その結果、がん性白血病細胞(CML 細胞)が無制限に増殖します。
CMLの最も一般的な治療はチロシンキナーゼ阻害剤(イマチニブなどのTKI)ですが、TKIは、CML細胞が分化して増殖する、いわゆる骨髄ニッチに存在するCML幹細胞には効果がありません。そのため、TKIによる治療を中止すると、CML幹細胞から再びCML細胞が増殖し、病気が再発します。
PAI-1阻害剤はCML幹細胞に作用してTKIの作用を増強し、CMLを完治させることが示されています。実際、PAI-1阻害剤RS5614をTKIと併用すると、骨髄中のCML幹細胞の数が著しく減少し、TKI単独と比較して生存期間が大幅に延長しました。TKIの開発によりCML患者の予後は大きく改善しましたが、CMLを治癒するには、長期にわたる高額なTKI治療を長期間続ける必要があります。また、TKIの長期継続使用による副作用も問題となっています。
RS5614は、多くのCML患者をできるだけ早期に無治療寛解(TFR)に導くことができる新しい作用機序を持つ安全な薬剤として期待されています。
- What were the results of the phase II studies in chronic myeloid leukemia (CML)?
-
2年以上TKI治療を受けているCML患者に、RS5614 120 mg/日を4週間投与し(TKIは12週間継続)、12週後のDMR(深い分子遺伝学的奏効:最高の治療効果)達成率を主要評価項目として評価した前期第II相医師主導治験が、東北大学、秋田大学、東海大学で実施されました。本試験には21名の患者が登録され、脱落者や中止者なく全例が解析対象となりました。主要評価項目の結果、21名中4名がDMRを達成し、12週時点での累積DMR達成率は20.0%でした(現在までのTKI単独治療3ヶ月時点での累積DMR達成率は、TKI単独治療(ヒストリカルコントロールと呼ぶ)の場合の平均は2.0%)。安全性評価では、解析対象となった21名全員に副作用は認められませんでした。
後期第II相試験では、CML患者を対象にTKIとRS5614(150 mg/日から開始し、180 mg/日まで増量可能)を併用投与し、RS5614投与開始後48週で累積DMRが33.0%(ヒストリカルコントロールの8.0%と比較して)に達することが期待できることを確認するとともに、RS5614とTKIの長期併用におけるRS5614の薬物動態および安全性を確認しました。その結果、33名中11名がDMRを達成し、48週時点での累積DMR達成率は33.3%でした(予想と同等のデータであったためPOCが確立しました)。安全性については、治験薬との因果関係が示唆される重篤な有害事象はありませんでした。
- Please tell us about the Phase III trial for chronic myeloid leukemia (CML).
-
Based on the results of the late Phase II study, a placebo-controlled, double-blind, investigator-initiated Phase III clinical trial to evaluate the efficacy of the combination of TKI and RS5614 in patients with chronic phase CML is underway in collaboration with 12 universities and medical institutions, including Tohoku University, Tokai University, and Akita University. This study was adopted by the Japan Agency for Medical Research and Development (AMED) under the Research Program of the “Practical Application for Innovative Cancer Therapy” in fiscal 2022 (Tohoku University is the representative research organization and Renascience participates as a sharing research organization). In November and December 2021, we held face-to-face consultations with the Pharmaceuticals and Medical Devices Agency (PMDA), and in May 2022, we submitted a notification of the clinical trial plan to the PMDA and started a multicenter Phase III study. Sixty (60) patients with chronic stage CML who had been treated with TKI for more than 3 years will be enrolled in the study, and the study will evaluate whether the combination of RS5614 significantly increases the maintenance rate of DMR for more than 2 years compared to TKI alone in 60 patients with chronic CML who have been treated with TKI for more than 3 years.
- What is the reason for developing the PAI-1 inhibitor in malignant melanoma?
-
Currently, there are four major cancer treatments: (1) surgery, (2) radiation therapy, (3) chemotherapy (anticancer drugs), and (4) immunotherapy. Immunotherapy is a treatment method that attacks cancers utilizing the body’s own immune system. Various immunotherapies have been proposed, but among the immunotherapies that have proven to be effective, immune checkpoint inhibitors, which inhibit the brakes of the immune system, are the mainstay. Since an excessive immune response is harmful, the body has mechanisms to suppress it. The molecules responsible for such a braking function are called immune checkpoint molecules. In fact, cancers abuse these immune checkpoint molecules to prevent the immune system from attacking against themselves.
Immune checkpoint inhibitors release this brake by blocking immune checkpoint molecules, thereby activating the immune response against cancers. We discovered that PAI-1 inhibits cancer immunity via immune checkpoint molecules. In animal model studies, we also found that malignant melanoma (melanoma), colorectal cancer, and other cancers regress in animals treated with RS5614, and that cancer immunity was synergistically and strongly enhanced when RS5614 was combined with an immune checkpoint inhibitory antibody.
We hope the checkpoint inhibitory activity of the PAI-1 inhibitor RS5614 is confirmed in the phase 2 study of malignant melanoma.
(What is malignant melanoma?)
Malignant melanoma is a type of skin cancer when melanocytes, skin cells that produce melanin pigment, which is related to skin color, become malignant. Among skin cancers, malignant melanoma has a high rate of metastasis and is considered to be extremely malignant. In Japan, the number of patients with malignant melanoma is as low as 0.6 per 100,000 people, but in the U.S. the number is 12.7 and in Australia 33.6, several tens of times higher than that of Japanese. Malignant melanoma is an extremely malignant cancer (5-year survival rate is about 50% when the size of the cancer exceeds 4 mm, 40% when there are metastases in the regional lymph nodes, and a few percent when there are distant metastases). Furthermore, the degree of progression of malignant melanoma in Japan is reported to be about three times higher than in the United States. This may be due to the fact that most malignant melanoma in Japan is of the acral lentiginous type, which is not major in Europe and the United States, making it difficult to respond to therapeutic agents.
The first treatment for malignant melanoma is surgical resection. However, the cancer is already advanced at the time of detection in many cases, and drug therapy (pharmaceuticals) is required for cases that are not radically resectable. Radiation therapy is not very effective for malignant melanoma. With the advent of antibody drugs (immune checkpoint inhibitors) such as nivolumab that target immune checkpoint molecules, drug therapy has made revolutionary progress. However, the response rate of nivolumab for malignant melanoma is 22.2% in Japan. Furthermore, the combination therapy of nivolumab and ipilimumab is approved for the patients refractory to nivolumab, and the response rate is 21% overseas and 13.5% in Japan. The combination therapy with nivolumab and ipilimumab causes serious side effects in more than half of patients, and the incidence of severe immune-related side effects that result in discontinuation of treatment is four times higher than that with the nivolumab therapy, requiring several months of hospitalization or interruption of cancer treatment. In addition, due to the challenge of high medical costs, there is a long-awaited need for a concomitant medication that can be orally administered differently from antibody therapeutics, have fewer side effects, and increase the response rate.
(Results of the Phase II study)
A Phase II investigator-initiated clinical trial to evaluate the efficacy and safety of the combination of RS5614, a PAI-1 inhibitor, and nivolumab, an immune checkpoint inhibitor, in the patients with malignant melanoma that is difficult to surgically resect was conducted in collaboration with six medical institutions including Tohoku University Hospital.
その結果、ニボルマブとRS5614の併用は、既存治療として報告されているニボルマブとイピリムマブの併用と同等以上の有効性を示しました(ニボルマブ+RS5614の奏効率は24.1%、ニボルマブ+イピリムマブの奏効率は13.5%)。ニボルマブとイピリムマブの併用は、重篤な免疫関連の副作用により安全性が懸念されていましたが、ニボルマブとRS5614の併用では問題となる副作用は認められませんでした。臨床試験報告書は2024年2月に完成しており、薬事承認申請に向けて次期フェーズ試験を準備する予定です。
- How will RS5614 change the treatment of malignant melanoma?
-
現在、ニボルマブとイピリムマブの併用は、ニボルマブに抵抗性の悪性黒色腫患者に対して承認され保険適用されているが、ニボルマブとイピリムマブの併用による重篤な副作用が問題となっている。日本臨床腫瘍研究グループ(JCOG)は、2021年4月から全国59施設でニボルマブとイピリムマブの併用療法の有効性を比較する第III相試験(JCOG2007)を実施し、ニボルマブとイピリムマブの併用群の患者の約7.4%(148人中11人)に治療関連死亡が見られ、予想以上に高い結果となったため、2023年3月30日に試験は終了した。このように、ニボルマブとイピリムマブの併用は、いくつかの種類の癌で問題となっている。
RS5614とニボルマブの併用は、ニボルマブに抵抗性の患者に対して、ニボルマブとイピリムマブの併用と同等以上の効果があり、RS5614とニボルマブの併用は、ニボルマブとイピリムマブの併用よりも安全です。免疫チェックポイント阻害剤単独では治療できない切除不能な悪性黒色腫に対する新規治療薬の開発は喫緊の課題です。ニボルマブとRS5614の併用は、免疫チェックポイント阻害剤単独療法では治療できない悪性黒色腫患者に対して、有効性が高く安全な薬物療法となることが期待されます。
- Is RS5614 useful in the treatment of other solid tumors?
-
動物モデルによる前臨床試験では、PAI-1阻害剤RS5614の経口投与により、大腸がんや肺がんだけでなく悪性黒色腫も退縮することが示されており、免疫チェックポイント阻害抗体との併用によりこの効果は大幅に増強されることが示されています。そのため、非小細胞肺がんおよび皮膚血管肉腫を対象とした第II相医師主導臨床試験を開始しています。
- What is the medical significance of the clinical trial for malignant melanoma?
-
PAI-1の発現が高いがんの多くは悪性度が高く、予後が悪いことが古くから報告されており、「PAI-1パラドックス」と呼ばれてきました。私たちは国内外の多くの大学との共同研究を通じて、がん細胞がPAI-1を産生し、PD-L1などの免疫チェックポイント分子の発現を高めることで免疫システムの攻撃を逃れていることを発見しました。動物モデルを用いた前臨床試験では、PAI-1阻害剤RS5614の経口投与により、悪性黒色腫、大腸がん、肺がんなどのがんが退縮することを実証しました。臨床試験では、手術による完全切除が不可能でニボルマブに抵抗性であった悪性黒色腫の患者29名のうち7名に、RS5614とニボルマブを8週間併用投与したところ、反応が確認されました。血液がんである慢性骨髄性白血病(CML)に対するRS5614の有効性は、すでに早期および後期の臨床試験で実証されています。フェーズII研究が終了し、フェーズIII試験が現在進行中です。私たちは、ヒトにおいて「PAI-1パラドックス」が癌治療において重要であること、PAI-1がいくつかの種類の癌の治療ターゲットであること、そしてPAI-1阻害剤が薬物治療として有効であることを確認しました。
- When will RS5614 be available for use in the medical field as a treatment for malignant melanoma?
-
第2相試験で有効性を確認できたことから、今後は規制当局と協議し、次相の臨床試験や薬事承認申請など、今後のロードマップを明確にしていきたいと考えています。また、レナサイエンスは医薬品の販売許可を持っていないため、他社との連携を通じて事業化への道筋を明確にしていきたいと考えています。
- What is the difference between RS5614, a PAI-1 inhibitor, and other immune checkpoint inhibitors?
-
従来の免疫チェックポイント阻害剤はいずれも抗体医薬品であり、入院や注射による投与が必要で、価格も高価です。また、既存の抗体医薬品はさまざまな副作用があることが知られています。RS5614は、自宅で服用できる安全性が高く利便性の高い医薬品となります。RS5614は抗体と異なり化学合成されるため、価格は抗体よりも低くなると予想されます。
- What is the reason for developing the PAI-1 inhibitor in lung cancer?
-
非小細胞肺がんの標準治療はプラチナ製剤を用いた化学療法と抗PD-1/抗PD-L1抗体を用いた免疫療法ですが、治癒する患者はごくわずかです。治療が奏効しない場合は、第2選択治療としてドセタキセルなどの化学療法が行われますが、生存期間は3か月と短く、第3選択治療が必要となります。しかし、第3選択治療に有効なものはほとんどなく、新しい薬剤が待望されています。本共同研究において、PAI-1が肺がんの進行・増殖に関与していること、抗PD-1抗体に耐性となったがん細胞が極めて高いレベルのPAI-1を発現していることを明らかにしました。実際、肺がんモデルマウスにおいて、抗PD-1抗体とPAI-1阻害剤の併用が抗PD-1抗体単独よりも高い抗がん活性を示すことを確認しました。これらの結果を踏まえ、広島大学病院を中心に、PAI-1阻害剤RS5614の非小細胞肺がんに対する有効性と安全性を確認する第II相試験を実施しています。
- What is the reason for developing the PAI-1 inhibitor in cutaneous angiosarcoma?
-
皮膚血管肉腫は稀な軟部腫瘍(国内で年間約300例)であり、腫瘍細胞にアポトーシス*を誘導するタキサン系抗がん剤が第一選択薬となっている。しかし、タキサン系抗がん剤で治療した皮膚血管肉腫患者90例の予後検討では、全生存期間は649日で治療効果は限定的であり、新たな治療薬の研究開発が急務となっている。PAI-1は主に血管内皮で産生されるが、我々は皮膚血管肉腫検体の解析において、PAI-1の高発現と予後不良に強い相関関係があることを見出した。PAI-1を高発現する癌細胞はアポトーシスに抵抗性であるという知見は、PAI-1阻害剤をタキサン系抗がん剤と併用することで、血管肉腫に対するタキサン系抗がん剤の治療効果を高めることができることを強く示唆している。そこで、タキサン系抗がん剤パクリタキセルが効かなかった皮膚血管肉腫の患者を対象に、PAI-1阻害剤RS5614の有効性を確認する第II相試験(医師主導治験)が東北大学を中心に実施されています。
※アポトーシス:細胞が損傷を受けて死滅するネクローシス(壊死)とは異なり、細胞自身の死のプログラムが活性化して細胞死に至る現象。
- What is the reason for developing the PAI-1 inhibitor in systemic scleroderma?
-
全身性強皮症(SSc)(日本の難病指定51)は、血管障害と皮膚や多くの臓器の線維化を特徴とする全身性自己免疫疾患であり、その病因はいまだに不明である。皮膚硬化、肺線維化(間質性肺疾患、ILD)、胃食道逆流症、心臓障害、手潰瘍などの症状を引き起こす難治性疾患である。
日本国内のSSc患者数は3万人以上と推定されています。ILDはSSc患者の死亡原因の30%以上を占める重篤な疾患です。ILDが直接の死因でなくても、線維化により肺機能が障害され、激しい咳や呼吸困難が生じ、日常生活に著しい制限が生じます。現在の治療法では効果が不十分な場合があり、自己免疫疾患の治療が進歩したにもかかわらず、SScでは全死亡原因の70%が疾患関連死であるのに対し、関節リウマチや全身性エリテマトーデスでは全死亡原因の10%未満を占めており、有効な治療法の開発が強く望まれています。
SSc は主に炎症、線維化、自己免疫に関連する血管損傷によって引き起こされるため、RS5614 はすべての症状を改善するため、SSc 症状の進行を抑制する可能性があります。実際、肺線維化を抑制する RS5614 の有効性は、SSc の動物モデルで実証されています。現在の SSc 治療薬の多くはステロイドや免疫抑制剤など強い副作用がありますが、RS5614 は安全性プロファイルが高いため、SSc に関連する ILD の治療薬として有用であると期待されています。
そのため、SSc-ILDに対するPAI-1阻害剤RS5614の有効性と安全性を調査する第II相試験が、東北大学病院を含む日本の複数の医療機関で実施されています。このプロジェクトは、日本医療研究開発機構(AMED)の資金提供を受けています。
- What is the reason for the PAI-1 inhibitor in novel coronavirus lung injury?
-
新型コロナウイルス感染症(COVID-19)の世界的な感染拡大は、大きな社会的課題となっています。感染者の約8割は軽症で済みますが、高齢者や基礎疾患のある患者を中心に、重症化すると重症肺炎や急性呼吸窮迫症候群(ARDS)を引き起こすことがあります。軽症の場合は自宅療養やホテル泊などで対応しますが、発症時は軽症であっても急激に重症化する患者もいるという問題があります。ワクチン接種やウイルス株(オミクロン株)の変異により、以前より重症化は抑えられていますが、重症化を引き起こすウイルス株のさらなる変異の可能性には注意が必要です。また、感染症法に基づく新型コロナウイルスの分類が「2類」から「5類」に引き下げられたことで、自宅療養や外来治療でさらに多くの患者が治療を受ける可能性もあります。当社は、肺炎を引き起こす新たな株が発生した場合に備え、できるだけ早く次の段階の臨床試験を実施できるよう準備を進めています。
肺炎の重症化を防ぐ薬、特に外来で処方され自宅で服用できる安全で簡便な予防・治療薬(内服薬)を開発することで、患者さんの延命のみならず、医療現場の負担軽減や医療資源の有効活用にも貢献したいと考えています。新型コロナウイルスによる重症肺炎の患者さんは、炎症や線維化などの病変が急速に進行し、血液凝固能が亢進するという特徴的な所見を示します。新型コロナウイルス肺障害の非常に特徴的な所見は、肺におけるフィブリン微小血栓、炎症、線維化です。
RS5614は炎症、線維化、血管損傷を抑制し、新型コロナウイルスによる肺障害の治療に効果がある可能性がある。
- What were the results of the Phase II studies of novel coronavirus lung injury?
-
2020年秋より前期第II相医師主導治験(オープンラベル)を実施し、2021年6月に治験報告書が完成しました。重大な副作用はなく、肺損傷で入院し治験薬を投与された患者26名全員が無事退院しました。
前期第II相医師主導臨床試験の結果を踏まえ、東北大学、京都大学、東京医科歯科大学、東海大学など国内20の大学・医療機関と連携し、新型コロナウイルス肺障害患者(中等症、入院患者)を対象にプラセボ対照後期第II相医師主導臨床試験を実施しました。本治験は、2021年3月にAMEDの「新興・再興感染症医療研究プログラム」(東北大学が代表研究機関、ルナサイエンスが分担研究機関)に採択され、2021年4月にPMDAとの事前協議に基づき治験計画を確定し、2021年6月に開始されました。感染者数の激減やオミクロン株の出現により、新型コロナウイルス肺障害(中等症、入院患者)の適格患者数が減少したため、治験は2022年10月末(最終的に75例が組み入れ)まで延長され、2023年4月に治験総括報告書がまとまりました。
主要有効性評価項目は両群間で統計的に有意な差は認められなかったが、RS5614群ではプラセボ群と比較して病状の悪化が軽減しており、特に比較的軽症の患者において有効性が示唆された。また、入院後3~5日間の酸素療法を必要とする患者の割合はRS5614群の方が低く、早期治療におけるRS5614の有効性が示唆された。また、RS5614群では肺炎の画像所見の改善が認められたが、プラセボ群では改善が認められなかった。副作用の発現率はRS5614群とプラセボ群で同程度であり、COVID-19関連肺障害患者に対するこの治験薬(RS5614)の安全性が確認された。
当社は、2020年12月25日に第一三共株式会社とRS5614の新型コロナウイルス肺障害およびその他の肺障害などの肺疾患への使用に関する優先交渉権に関するオプション契約を締結しました。2022年11月には、新型コロナウイルス肺障害だけでなく抗がん剤治療に伴う間質性肺炎に対するRS5614の有効性を確認する臨床試験の実施を視野に入れ、オプション期間を2025年3月まで延長する覚書を締結しました。
- Is PAI-1 inhibitor effective for lung injuries other than novel coronavirus lung injury?
-
非臨床試験では、当社のRS5614が血栓形成、炎症、線維化を抑制することが示されており、間質性肺炎に効果がある可能性が示唆されています。肺障害はウイルスだけでなく、抗がん剤、自己免疫疾患、原因不明の特発性疾患など、さまざまな原因で引き起こされるため、これらの肺障害に対する有効性を評価する臨床試験を実施します。
その一環として、京都大学医学部附属病院呼吸器内科と、特発性間質性肺炎の急性増悪を対象とした臨床試験の実施に向けた連携を開始しました。特発性間質性肺炎の急性増悪は、特発性間質性肺炎による死亡例の約 40% を占める予後不良の疾患です。また、第一三共株式会社との契約を延長し、抗がん剤治療などに伴う間質性肺炎に対する本剤の有効性を確認する臨床試験の実施も行っています。さらに、全身性強皮症に伴う間質性肺炎に対する PAI-1 阻害剤 RS5614 の有効性と安全性を検討する第 II 相試験が、東北大学病院を含む国内の複数の病院で実施されました (国立研究開発法人日本医療研究開発機構 (AMED) の支援による)。
- Is the PAI-1 inhibitor effective in preventing aging?
-
私たちは、米国ノースウェスタン大学と共同で「PAI-1と老化」に関する研究を行っています。
生物の細胞は細胞老化という現象により無制限に増殖することができません。この現象にはゲノムのテロメア長の短縮とp53などの細胞老化因子が関係しています。老化細胞はp53に加えてPAI-1の発現が非常に高いことが分かっています。実際、p53やPAI-1を抑制することで細胞老化現象を抑制できることが明らかになっています。PAI-1の発現は細胞だけでなく老化組織や個体(早期老化の代表的な病態であるクロトーマウスやウェルナー症候群のヒト)でも高いことが報告されています。老化の代表的なモデルであるクロトーマウスでは、PAI-1の発現や活性を遺伝子やタンパク質レベルで抑制することで、老化の主要な症状がすべて改善されることが示されています。さらに、中西部に住むキリスト教の一派であるアーミッシュの人々を対象とした研究では、PAI-1遺伝子を持たない人々は持つ人々よりも10年長生きすることがわかりました。また、この遺伝子が欠乏している人は糖尿病などの病気にかかりにくいこともわかりました。
これらの事実は、2017年11月にニューヨークタイムズ紙など多くの新聞で報じられた。研究の主任研究者でノースウェスタン大学医学部の教授である同氏は、「彼らは単に長生きしているだけではなく、より健康に暮らしている」と語り、「これが理想的な長寿の形だ」と付け加えた。このヒトでの疫学研究は、細胞やマウスでの実験結果と一致しています。加齢とともに、がん、血管(動脈硬化)、肺(肺気腫、慢性閉塞性肺疾患)、代謝(糖尿病、肥満)、腎臓(慢性腎臓病)、骨・関節(骨粗鬆症、変形性関節症)、脳(脳血管疾患、アルツハイマー病、認知症)などの疾患が発症します。興味深いことに、これらの疾患の組織ではPAI-1の発現が極めて高くなっています。さらに、これらの疾患の動物モデルにPAI-1阻害剤を投与すると、症状が著しく改善することが確認されています。
最近、老化細胞が免疫のブレーキ役(免疫チェックポイント分子)のタンパク質PD-L1を発現し、免疫からの攻撃を逃れていることが報告されています。免疫チェックポイント分子を阻害する治療薬(免疫チェックポイント阻害剤)は、老齢マウスや生活習慣病マウスの免疫系を活性化させます。活性化された免疫系は老化細胞を排除し、マウスのさまざまな臓器や組織の老化や生活習慣病を改善します。
我々は、PAI-1ががん細胞における免疫チェックポイント分子の発現に関与し、がん細胞の増殖を促進すること、また、我々のPAI-1阻害剤が免疫チェックポイント阻害作用を有することを発見しました。つまり、PAI-1はがんや老化を促進しており、我々のPAI-1阻害剤はがんやその他の老化関連疾患に効果がある可能性があります。
これらは、PAI-1 と老化に関して明らかになった興味深い発見のほんの一部です。ただし、PAI-1 阻害剤が老化防止に効果があるかどうかは不明です。現時点では、これを証明する臨床試験は実行不可能だからです。
- What is the status of clinical trials for premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD)?
-
RS8001は、PMS/PMDDを対象とした第II相医師主導治験を、近大、東北大、東京医科歯科大学、東京女子医大と共同で実施しています(プラセボリードイン*二重盲検プラセボ対照3群比較試験、目標症例数105例)。本治験は、令和元年度AMED「医療研究開発革新基盤創成事業(CiCLE)」(代表研究機関:ルナサイエンス)に採択されました。
治験は当初予定の2021年2月から前倒しで2020年11月に開始しましたが、新型コロナウイルス感染症拡大の影響により来院患者数が減少したため、2021年度は新たに治験実施施設を2カ所追加し、院内でのポスターや啓発冊子の作成、治験責任医師による薬剤師向けWebセミナーの実施などにより、患者の登録促進を図りました。2022年11月には治験実施施設を3カ所追加し、ボランティアパネルの活用や治験責任医師による公開講座の開催などの施策を講じました。その結果、2023年9月に目標登録数を達成しました。AMEDは中間評価において事業継続を決定し、2024年6月に報告書を取りまとめました。今後の開発の方向性については、現在AMEDと協議中です。
※プラセボ導入法:プラセボには有効成分は含まれませんが、心理的な効果(プラセボ効果)により病気の症状が改善する可能性があるため、有効成分投与前に一定期間プラセボを服用していただき、プラセボ効果が大きい被験者には試験への参加を求めない試験デザインを採用しています。
- What is SaMD utilizing AI for supporting diabetes treatment?
-
糖尿病では、血糖値を厳格にコントロールし、糖尿病合併症を予防するためにインスリン療法が必要です。しかし、インスリンの安全な投与量の範囲は狭く、過剰投与は低血糖を引き起こすため、患者ごとに最適な種類と投与量を選択する必要があります。一方、糖尿病専門医は医師全体の2%未満であり、地理的に偏在しているため、糖尿病患者は必ずしも糖尿病専門医である主治医ではなく、非糖尿病専門医に診てもらうのが現状です。
そこで我々は、東北大学、日本電気株式会社と共同で、糖尿病専門医以外の医師が糖尿病専門医レベルのインスリン治療を行うことを支援するAI「DM-SAiL(SAiLはSkill Acquisition Learningの略)」の開発に取り組んできました。東北大学病院に入院した約1,000名の患者データ(約108万項目)の解析を完了し、糖尿病専門医の処方量との誤差2単位程度のインスリン投与量を予測するAIの開発に成功しました。東北大学病院の入院患者の正解率は全体で約90%と非常に高く、糖尿病専門医の処方量との誤差率(インスリン単位の差)は超速効型・持効型ともに0.65~0.95単位でした。現在、このSaMDをクラウド上で利用する仕組みをNEC Solution Innovatorと共同で開発しており、デモシステムの開発も完了しています。
2022年4月にAMED「令和4年度医工連携事業化促進事業(中小企業開発・事業化支援)」に採択され(当社が代表研究機関)、実用化に向けて開発を進めています。2022年12月にPMDA開発前相談が完了、2023年5月にPMDAプロトコル相談(事前相談)が完了、実用化に向けて開発を進め、2024年8月に臨床性能試験を開始する予定です。
- What is SaMD utilizing AI for supporting maintenance hemodialysis?
-
慢性腎不全患者は、機能低下した腎臓の代わりとして老廃物を除去するため、生涯にわたり週3回の血液透析を受けます。脱水が不十分だと心不全や高血圧などの心肺機能障害を引き起こし、脱水が過剰だと透析中の低血圧や気分不良、意識消失などの有害事象を引き起こします。また、不適切な水量設定による水分除去不足や過剰は有害事象を引き起こす可能性があり、患者対応を強いられる医療従事者に大きな負担をかけています。
安全な透析を実現するために、私たちは東北大学、日本電気株式会社と共同で、適切な総除水量を予測するAI(Dual-Channel Combiner Network、DCCN)の開発に取り組んできました。DCCNは、聖路加国際病院や民間透析施設から取得した725,000件の透析記録(患者情報、透析情報、検査情報)を学習し、患者の過去5回の透析記録と透析当日の透析前データに基づいて目標除水量を予測します。現在、透析中の急激な血圧低下(20mmHg未満)をAUC 0.91の精度で予測し、腎臓内科医が経験的に設定した総除水量と「コップ1杯」程度の誤差で総除水量を予測することが可能です。
2023年4月にPMDAとの開発前相談を完了し、実用化に向けて開発を進めております。
本プロジェクトは、2023年2月にAMED「新たな医療機器開発研究」プログラムに採択され、2021年5月にニプロ株式会社と本AIの開発に関する連携契約を締結しました。また、2023年12月には東レ・メディカル株式会社と共同で、血液透析における除水量や血流量を制御できるAI搭載血液透析医療機器の開発を開始しました。
- What is SaMD utilizing AI for diagnosis of swallowing dysfunction?
-
加齢に伴う口腔機能の低下(オーラルフレイル)は、放置すると摂食障害や構音障害(言語障害)などの身体的・社会的機能障害や全身の筋力低下(フレイル)につながるため、早期診断と適切な治療が重要です。高齢化社会では口腔機能低下の一つである摂食・嚥下障害が増加しており、死因とされる肺炎の約70%は誤嚥が原因であると報告されています。誤嚥性肺炎を予防するには、嚥下機能障害の早期発見とリハビリテーションなどの治療介入が重要ですが、現状では嚥下内視鏡検査や透視検査などの嚥下評価方法しかなく、患者に負担がかかります。
嚥下と発話に用いられる器官は、舌、口腔、咽頭など共通する部位が多いことから、会話から嚥下機能を評価できる可能性に着目し、会話中の音声データから嚥下機能障害を評価できるAIの開発に取り組んでいます。東北大学の複数の部局(耳鼻咽喉科、歯学、リハビリテーション医学、大学院医工学研究科)や日本電気株式会社と連携し、東北大学病院嚥下障害治療センターを受診する患者の発話音の全周波数を、時系列データの解析に特化したAIエンジン(時系列モデルフリー解析)で解析し、健常者の音声のベースライン(性別、年齢、個人差など)を確認したり、健常者と患者の発音の違いを検出したり、嚥下機能の低下を診断したりするAIを開発することができました。
今後は、嚥下機能が低下した高齢者のデータを学習させ、実用化に向けたAIの開発を進めていきます。このプログラム医療機器が実用化されれば、誤嚥性肺炎を発症する恐れのある嚥下機能が低下した患者を、容易かつ早期に診断できるようになります。2023年3月には東北大学と共同で知的財産権に関する特許出願を行いました。
- What is SaMD utilizing AI for supporting respiratory function test?
-
スパイロメトリーは、被験者が吐き出す息の量と吐き出す時間を測定する呼吸機能の生理学的検査であり、慢性閉塞性肺疾患(COPD)やその他の肺疾患の診断に重要な検査ですが、広く普及していません。被験者(患者)の協力(呼吸努力)が必要なほか、検査が正しく行われたかどうかの判断や出力(フローボリューム曲線)の解釈が専門医以外では難しいためです。専門医以外でも結果を容易に解釈できるシステムの開発は、呼吸器疾患の診断と早期治療のための重要な医療課題とされています。
当社は、京都大学、NECソリューションイノベータ株式会社と共同で、フローボリューム曲線を判読するAIの開発を進めており、約1,900例の医療データを取得しており、実用化に向けた開発を進めています。2020年7月にChest MI Inc.と協業・事業化契約(ライセンス契約)を締結し、2021年10月と2023年6月にマイルストーンペイメントを受領しました。
- What other projects are you working on to develop SaMD utilizing AI?
-
重点領域の一つである女性疾患に関する取り組みとしては、東北大学と共同で乳がんの病理画像から病変を検出するAIの開発を進めてきました。病理画像を用いた検証では、検出モデルを良性、非浸潤がん、浸潤がんの3クラスと良性、悪性の2クラスに分類し、それぞれ88.3%と90.5%の診断精度を達成しました。今後は乳がん領域において「術中病理標本」でのAI診断に取り組む予定です。
また、加齢に伴う疾患に関連した取り組みとして、東北大学と共同で、心臓埋め込み型デバイスの情報を活用して不整脈や心不全の発生を予測するAIの開発に取り組んでいます。
2022年9月にハイレックスコーポレーション、ハイレックスメディカルと連携協定を締結し、ハイレックスメディカル、東北大学と連携し、補助人工心臓における血栓発生を予測するAIの開発に取り組んでまいります。
- What kind of collaborations do you conduct with NEC Corporation and NEC Solution Innovator, Ltd.?
-
AIを活用した医療機器ソフトウェア(SaMD)には、AIをコア技術として、医療現場でAIを稼働させるシステムの開発が必要です。解決したい医療課題や活用する医療データの種類に応じて、最適なAIアルゴリズムを選択する必要があります。当社は、NEC株式会社より基本的なAIアルゴリズム(エンジン)のライセンスを取得し、医療現場の医療データや医師のアドバイスをもとに、医療向けにカスタマイズしています。医療用AIのシステム開発は、NECソリューションイノベータ株式会社(NES)に委託しています。
- What is a disposable ultrafine endoscope?
-
腹膜透析患者の腹膜内には透析液を注入するためのチューブが留置されます。私たちは、この細いチューブに挿入する極細内視鏡(直径約1mm)を、開腹手術や腹腔鏡手術をせずに非侵襲的に腹腔内を観察する装置を東北大学、順天堂大学、東京慈恵会医科大学と共同で開発しました。
2022年8月にファイバースコープ本体がPMDAに承認申請され、同年12月に厚生労働省より薬事承認されました。
当社は、2022年9月に株式会社ハイレックスコーポレーションおよびその子会社である株式会社ハイレックスメディカルと、ガイドカテーテルを含む医療機器の開発に関する協業契約を締結しました。
当社は、2024年5月にハイレックスメディカル株式会社と腹膜透析を含む医療用途向け本内視鏡のライセンス契約を締結しました。
- What is the diagnostic for phenylketonuria?
-
フェニルアラニンは体内のタンパク質を構成するアミノ酸の一つで、体内の酵素によってチロシンという別のアミノ酸に代謝されます。フェニルケトン尿症は、先天的に酵素の働きが低いためにフェニルアラニンが代謝されずに体内に蓄積する病気で、小児難病に指定されています。適切な治療を施さないと、知的障害やけいれんなどの重篤な症状を引き起こすことがあります。1977年に集団出生後スクリーニングが導入され、現在では罹患児のほぼ全員が早期発見されるようになりました。
しかし、罹患児は適切な食事でフェニルアラニンを制限する必要があり、医療機関での定期的な検査が必要ですが、数ヶ月に一度の採血ではきめ細かな食事管理ができません。糖尿病患者用の自己血糖測定器のような家庭で利用できる血糖測定システムもないため、フェニルアラニン食の自己管理は現状困難です。
我々は東北大学と共同で、血中フェニルアラニン濃度を自宅で簡便かつ正確に測定できるシステムの開発を進めており、この新しい検査システムをキット化し、保険償還による自己管理につなげることを目指しています。糖尿病患者の自己血糖コントロールのように、自宅でいつでも自己測定できれば、フェニルケトン尿症患者のきめ細かな食事管理が可能になります。
- What is important in the development of a medical device and software as a medical device?
-
優れた技術であっても、医療現場の課題やニーズに合致しなかったり、医療現場の仕様に適していなかったりして、医療への応用(実装)が難しいケースが多くあります。技術を保有する多くの企業がこの課題に直面しています。当社は、医療現場のニーズを起点に課題解決を図り、医療現場での最終製品をイメージしてプロセスを最適化する「バイオデザイン」の考え方に基づき、医療機器や医療機器としてのソフトウェアの開発に取り組んでいます。
Financials
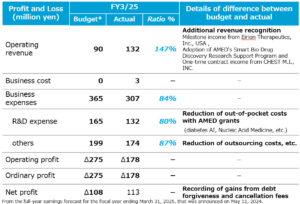
- How were your full-year results for the fiscal year ending March 31, 2025?
-
For the full fiscal year ending March 2025, we achieved operating revenue of 132 million yen and net income of 113 million yen. In terms of revenue, in addition to contract fees with companies, we received a grant from the Japan Agency for Medical Research and Development (AMED), and additional milestone income was recorded, resulting in 147% of the plan.
In terms of expenses, the amount of operating loss was reduced compared to the initial plan by utilizing public funds from AMED in the development of pipelines such as medical devices for diabetes treatment support programs and chronic myeloid leukemia (CML).
Although we reduced our own research and development expenses, as a result of implementing efficient research and development activities, which are our strength, the initial target for pipeline development (number, stage) is progressing as planned.
In addition, as extraordinary income, we recorded cancellation fees associated with the termination of the license agreement with Baxter for disposable ultra-thin endoscopes and debt forgiveness gains associated with the reduction of debt for AMED’s CiCLE program, resulting in net income of 113 million yen.
- When do you announce your financial results?
-
第1四半期:8月中旬、第2四半期:11月中旬、第3四半期:2月中旬、決算発表:5月中旬。
以下のページをご参照ください。
- When is your business year and fiscal year end?
-
会計年度は4月1日から翌年3月31日までで、毎年3月に終了します。
- Where can I find the financial results?
-
以下のページをご参照ください。
- Where can I check past performance?
-
以下のページをご参照ください。
- Do you have a timeline for turning to profitability at this point?
-
安定的に黒字化できる時期を明言することは難しいですが、数年以内には単年度黒字化できる可能性があると考えています。その理由の一つは、パイプラインの導出収入(契約一時金、開発段階に応じたマイルストーン、製品売上に応じたロイヤリティ等)にあります。
Stock/Shareholder
- Who should I contact regarding shareholder procedures?
-
株式に関する各種手続きに関するお問い合わせは、下記までお願いいたします。
三井住友信託銀行株式会社 証券代行部
電話番号 0120-782-031(フリーダイヤル)
※証券口座をお持ちの場合は、お取引のある証券会社にお問い合わせください。
- What is the status of your major shareholders?
-
以下のページをご参照ください。
- Who should I contact for IR inquiries?
-
お問い合わせは下記ページよりお願いいたします。
いただいた質問の多くは、当社のウェブサイトの FAQ を通じて公開します。